Senegal transforms the childbirth experience through WHO‑recommended care models
In less than a decade, Senegal has reduced its maternal mortality rate by more than 50%, from 392 deaths per 100 000 live births in 2015 to 153 in 2023. Behind this progress, however, a more complex reality persisted: in many health facilities, women continued to experience childbirth marked by fear, lack of information and impersonal health care.
Tina, 32, a mother of three, remembers her first two deliveries as moments filled with anxiety: limited explanations, minimal communication with health staff and a feeling of being alone in the face of pain. “They were very difficult births for me. After my first experience, I carried that fear with me during every pregnancy,” she says.
Tina’s experience is far from unique. Her story reflects the reality faced by many women in Senegal, despite the significant progress made in maternal health outcomes.
To address these challenges and ensure that every birth is a positive experience, the Ministry of Health and Public Hygiene (MSHP), with support from World Health Organization (WHO) and a major donor, introduced the Respectful Maternity Care (RMC) initiative. This approach aims to place dignity, emotional well‑being and women’s choices at the centre of health care practices, going beyond survival alone.
Respectful Maternity Care is built on three essential pillars: birth preparedness for pregnant women; use of the Labour Management Guide by health workers and psychological support for women throughout pregnancy and during childbirth.
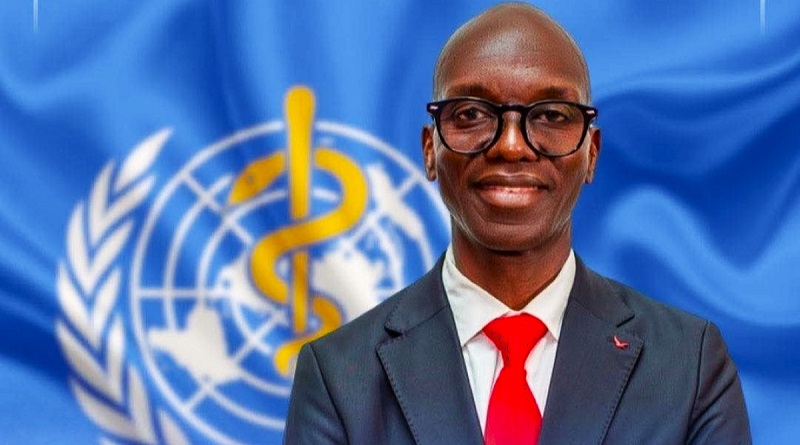
“The goal goes far beyond survival,” explains Dr Ousmane Dieng, Maternal and Newborn Health Expert at the WHO Country Office in Senegal. “It is about offering every woman a positive experience in which she feels heard, informed and fully involved in her childbirth.”
At the Yeumbeul Reference Health Centre, in the suburbs of Dakar, the RMC approach has been implemented for two years. Every other Wednesday, women who are six months pregnant or more meet with midwives for birth preparation sessions. These sessions follow a comprehensive curriculum covering the biological aspects of pregnancy, danger signs, simulations of childbirth positions, breathing techniques, mobility exercises and newborn care.
Following a pilot phase conducted between 2019 and 2023 at the Yeumbeul reference hospital, the initiative has been scaled up since November 2023 to all health facilities in the health district of the Yeumbeul North and South municipalities. To support effective implementation, 45 midwives in the district have been trained in this approach and more than 430 women have received support.
For her third pregnancy, Tina participated in the programme. Aware of her previous experiences, the midwives reassured her and taught her techniques to better manage pain, understand the different stages of labour, and prepare mentally for childbirth. Sitting in the postnatal ward of the Yeumbeul hospital, Tina gently cradles her newborn as she recounts her story. “During labour, I was assisted by the same midwife who had guided me during the preparation sessions. Together, we practiced the exercises again and it allowed me to experience the birth of my son differently—with more confidence and calm,” she says.
This birth‑preparation approach, combined with the use of the new Labour Management Guide, helps reduce preventable maternal and neonatal deaths. The guide simplifies the monitoring of labour and enables early detection of complications, while promoting a more humane approach to care. WHO has supported the training of 2700 midwives in its use across the country.
“Before, midwives were very focused on complex charts, sometimes at the expense of continuous support,” acknowledges Dr Alassane Tall, Head of the Gynecology Unit at Yeumbeul Hospital. “Today, the tool is more intuitive and allows more time for listening to women and adapting care accordingly.”
To support this shift, WHO has also assisted in the adaptation and dissemination of a complementary module on stress management for midwives, with 235 health professionals trained. Beyond technical procedures, the emphasis is placed on communication, adaptation to each woman’s needs and the well‑being of midwives, thereby strengthening the quality of care.
“The preparation sessions with pregnant women allow us to better anticipate their needs and build a relationship of trust by integrating listening and emotional support into care, beyond technical acts alone,” says Gnima Sonko, Senior Midwife at the Yeumbeul Health Centre, trained with WHO support. “The modules focused on strengthening our own mental health help us work with greater peace of mind, which directly improves the quality of support we provide to pregnant women.”
This integrated approach is transforming the childbirth experience. “Every woman deserves to experience childbirth in dignity and safety. This is a fundamental right, not a privilege,” stresses Dr Michel Yao, WHO Representative in Senegal. “Collaboration between the Ministry of Health, health districts and WHO is essential to scaling up these good practices.”
For Tina, the change was tangible: “My baby was born in joy, not fear. I am leaving with a light heart.” A testimony that shows how humane health care transforms lives — one pregnancy, one birth, one family at a time.